


|
Physiotherapy and Parkinson's Disease Introduction Parkinsonís Disease is a movement disorder, which may affect balance, posture and performance in daily activities such as turning in bed, sit to stand, walking and hand dexterity. It may have a major impact on a personís work, family and leisure activities. However statistics show that referrals to physiotherapy are low and have changed little in the past twenty years, despite the fact that physiotherapy addresses many of the core areas outlined above. |
| |
 How can Physiotherapy Help a Person with Parkinsonís Disease? Symptoms a person may experience include some or all of the following:
which can affect everyday physical activities such as, moving in bed, hand dexterity, walking, working, and recreation. Over time, secondary problems may arise such as loss of flexibility, weakness, postural change, discomfort and pain, further affecting movement and function. Physiotherapy aims to promote and maximise a personís independence and quality of life through rehabilitation, education and support for the individual and their family. When Should I See a Physiotherapist? Following diagnosis, early referral to physiotherapy is recommended. The individual has the opportunity to discuss any concerns or worries relating to the condition and his symptoms. Early assessment allows the physiotherapist to address current problems and to identify any potential ones. A treatment program can be devised specifically for your needs. He/she can give practical advice on physical management of the condition, aids and adaptations that may help in the home or at work, and can provide information on services available in the community, including information on specific support groups. Early referral also provides baseline objective levels of performance. Any change in the person's condition or functional ability can be promptly addressed throughout the course of the condition. What Should I Expect on Initial Contact with the Physiotherapist? The Physiotherapist will carry out a comprehensive assessment, which will include a detailed account of your history relating to diagnosis, history of symptoms, i.e. stiffness, fatigue, pain and how they affect everyday activities in the home, at work and social activities. She will ask about current medication and past medical history. The assessment will also include a physical examination, an analysis of posture, body movements and performance of functional activities, e.g. rolling, walking indoors / outdoors, balance activities, and climbing stairs. From this comprehensive examination, the physiotherapist will discuss the current findings with you, identify potential problems and decide on the most appropriate course of action. A rehabilitation programme is then devised to address your specific needs. How Long Will I Need to See a Physiotherapist? This will really depend on each individual presentation and the findings upon examination. The physiotherapist may recommend any of the following:
It is often the case that the physiotherapist will recommend one or more of the above, given the nature of the condition and the changing needs of the person. It is recommended that your condition and progress are monitored on a regular basis through regular reviews and intervention as required to achieve your optimal functional potential.
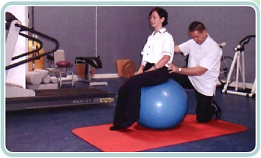
What does Physiotherapy Treatment Involve? Treatment is very dependent one's symptoms. It may be Hands on work, i.e. stretching, mobilising tissues, massage, or it may consist of various forms of exercise, addressing posture, balance, flexibility and strength. Usually a combination of both is needed. Treatment may also include teaching of movement strategies. This involves learning new techniques to perform a functional movement - usually automatic movements (e.g. turning in bed, standing up, stepping, turning, walking through doorways) which can become increasingly difficult with this condition. If pain is a problem then an assessment of the particular area of your body may be needed to identify the faulty tissues - joint, muscle, nerve or ligaments. In PD, common areas of pain are the neck and lower back. Your postural habits, body movements and daily activities are also assessed. Treatment may include manual therapy for the appropriate structures, exercise, and advice regarding posture and movement. What Type of Physiotherapy Treatment is Best? In the last few years a professional body in England has reviewed the evidence in relation to best-practice treatment for Parkinsonís disease. The findings suggest that further research is needed! However studies they did look at showed that exercises such as stretching, strengthening, balance re-education, breathing control, relaxation and aerobic exercise i.e. cycling, walking can all have a positive effect on a personís well being and help to promote functional independence. It has also been suggested that exercise is most effective whilst maintaining an optimal drug regime. Some studies looked at carrying out exercise classes over a certain period of time. Many programmes included exercises for improving strength and flexibility in the head and neck, trunk and limbs together with exercises for balance, posture, speech and breathing control, relaxation, and walking re-education. What was highlighted was the difficulty a person might have of continuing with these exercises once the class was completed. To promote compliance it was suggested that regular home visits together with top-up programmes were needed. What are the Benefits of Individual Therapy and Group Therapy? To have a clear understanding of the personís problems, a comprehensive assessment on a one to one basis with the physiotherapist is essential. Most people like to have individual treatment with a physiotherapist where they can discuss their personal problems privately and where personal needs are addressed and progress is monitored closely through personal supervision. A structured class has the advantage of providing motivation, social contact, camaraderie and it can be fun. What are the Benefits of Exercise? There are many benefits of exercise. Exercise:
Exercise will not change the course of the condition, but it may promote your level of wellbeing and quality of life and help counteract the effects of the symptoms. Movement Patterns The basal ganglia is involved in complex automatic movement patterns. As mentioned, in Parkinsonís disease a person may have difficulty performing such automatic movements as rolling, walking, or sit to stand. To execute the movement, sequence cues may link components of the movement. There are four possible cues:
If we take an example of freezing when walking, we may help overcome the freezing either by use of:
Thinking of the sequence of the movement we want to perform prior to carrying it out may help. Research has shown that there is greater improvement in performance, over a longer period of time, if movement strategies are incorporated into the rehabilitation program, as compared to when they are not. They also suggest that these compensatory movement strategies should be performed at peak medication dose. The Role of Carers in Rehabilitation Involvement of carers is vital, as they can provide much information relating to problems faced at home. The physiotherapist can give practical advice on the most effective ways to stretch, and how to assist with movements such as transfers and walking. How Can I Access a Physiotherapist? A person can access community and outpatient physiotherapy services in Ireland through referral from a GP, Consultant e.g. Neurologist, Geriatrician or Physician. Alternatively an individual can refer himself to a private physiotherapist, preferably one who specialises in the treatment of Neurological conditions. Some physiotherapists will provide private treatment at home as well as in a clinic. The advantage of seeing a physiotherapist in hospital / clinic is the available space and the accessibility to various pieces of equipment. When treating in the home the physiotherapist has the opportunity to understand the everyday movement problems you face and provide practical advice and support. She also has the opportunity to address the problems you encounter in the community, e.g. freezing in local shops, difficulty getting on /off the bus, or crossing the road. How Do We Evaluate if Physiotherapy is Effective? One of the main ways is obviously to ask your opinion, i.e. to fill in a questionnaire, to note what changes you feel each day. We may also use visual observation of functional activities by photography or video analysis of walking. Time tests provide objective measures. The most common ones include:
| ||
